By Nancy Morgan, RN, BSN, MBA, WOC, WCC, DWC, OMS
Each issue, Apple Bites brings you a tool you can apply in your daily practice. Here’s an overview of performing a comprehensive skin assessment.
In the healthcare setting, a comprehensive skin assessment is a process in which the entire skin of a patient is examined for abnormalities. It requires looking at and touching the skin from head to toe, with a particular emphasis on bony prominences and skin folds. Comprehensive skin assessment is repeated on a regular basis to determine whether changes in the skin’s condition have occurred. The goal of a skin assessment is to identify problem areas promptly for treatment and prevention.
The answers to the questions below will help ensure your skin assessments are truly comprehensive.
When and how often should I perform a comprehensive skin assessment?
• As soon as possible but within 8 hours of admission (or first visit in community settings)
• Ongoing based on the clinical setting and the patient’s degree of risk
• More frequently in response to any
deterioration in the patient’s overall condition
• Before the patient’s discharge
What are key points I should remember?
• Take advantage of every patient encounter to evaluate part of the skin. Each time the patient is repositioned is an opportunity to conduct a brief skin assessment.
• Ensure adequate light. Use natural or halogen light, not fluorescent. Fluorescent light imparts a bluish tone to dark skin, making it harder to see skin changes.
• Use an additional light source, such as a penlight, to illuminate hard-to-see skin areas, such as the heels or sacrum.
• Inspect the skin under and around medical devices (e.g., tubing, splints, compression stockings) at least twice daily for signs of pressure-related injury on the surrounding tissue. Conduct more frequent assessments in patients vulnerable to fluid shifts and in those exhibiting signs of localized or generalized edema.
• Remember that you can combine the skin inspection with other assessments.
How do I do the assessment?
• Explain to the patient and family that you will be looking at his or her entire skin and explain the purpose—to identify potential problems.
• Perform the assessment in private.
• Minimize exposure of body parts during the skin assessment.
• Conduct a systematic, head-to-toe assessment, with particular focus on skin overlying bony prominences, such as the sacrum, ischial tuberosities, greater trochanters, and heels. Check skin folds, between fingers and toes, and under and around medical devices for skin integrity.
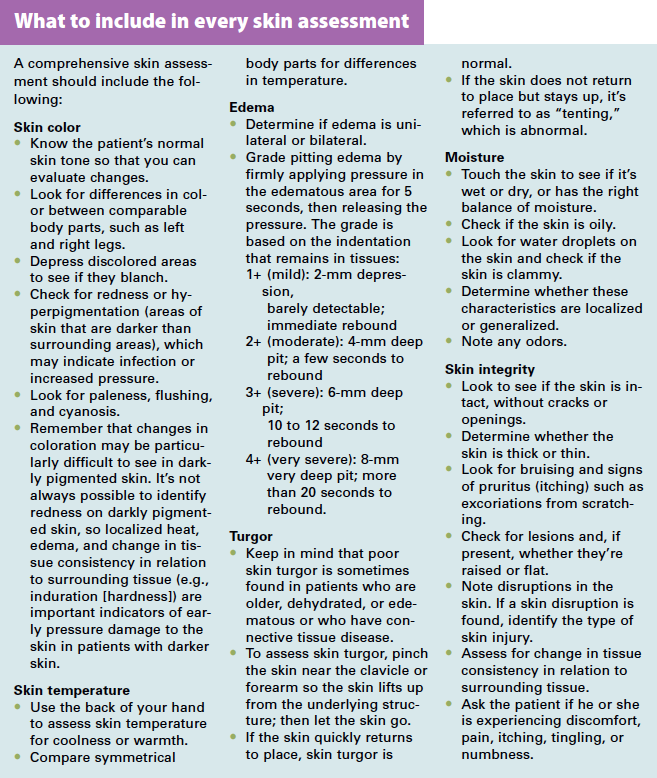
• Include the factors detailed in What to include in every skin assessment.
• Document the findings of all skin assessments for communication and tracking. You can download a Weekly skin assessment form here. (See Weekly skin assessment.)
Protecting your patients
A comprehensive skin assessment is essential to detecting early signs of skin breakdown. By using the techniques in this article, you can protect your patients from harm and ensure they receive prompt treatment for identified problems.
Selected reference
Preventing Pressure Ulcers in Hospitals: A Toolkit for Improving Quality of Care. AHRQ Publication No. 11-0053-EF, April 2011. Agency for Healthcare Research and Quality, Rockville, MD.
Nancy Morgan, cofounder of the Wound Care Education Institute, combines her expertise as a Certified Wound Care Nurse with an extensive background in wound care education and program development as a nurse entrepreneur.
Information in Apple Bites is courtesy of the Wound Care Education Institute (WCEI), © 2015.
DISCLAIMER: All clinical recommendations are intended to assist with determining the appropriate wound therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patients’ attending physicians. Nothing in this information shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Individuals should contact their healthcare providers for medical-related information.